THE ROLE OF ENDOSCOPY IN DIAGNOSING GERD
7/2/2025 3:48:54 PM
This article has been medically reviewed by Dr. Nguyen Huy Bang, MD, PhD – Specialist in Gastrointestinal Endoscopy.
1️⃣ GASTROESOPHAGEAL REFLUX DISEASE (GERD) AND THE ROLE OF GASTROINTESTINAL ENDOSCOPY
Gastroesophageal reflux disease (GERD) is a very common condition that occurs when stomach acid flows back up into the esophagus, causing symptoms such as heartburn, acid regurgitation, bloating, or a burning sensation in the chest. Although common, GERD is not always easy to diagnose because its symptoms can easily be confused with those of other digestive disorders. If left untreated, GERD can lead to serious complications such as esophagitis, esophageal stricture, or even esophageal cancer.
According to the Lyon Consensus 2.0, endoscopy not only helps detect esophagitis, Barrett's esophagus, or strictures caused by reflux but also plays a key role in confirming, supporting, or ruling out GERD with high accuracy.
As per the latest guidelines, a precise GERD diagnosis requires clear evidence from endoscopy or 24-hour esophageal pH monitoring, combined with the patient’s corresponding clinical symptoms.
2️⃣ THE ROLE OF ENDOSCOPY IN DIAGNOSING GERD
⭐ Confirming the diagnosis:
An upper gastrointestinal (GI) endoscopy (esophagogastroduodenoscopy) can reveal clear signs of GERD, such as:
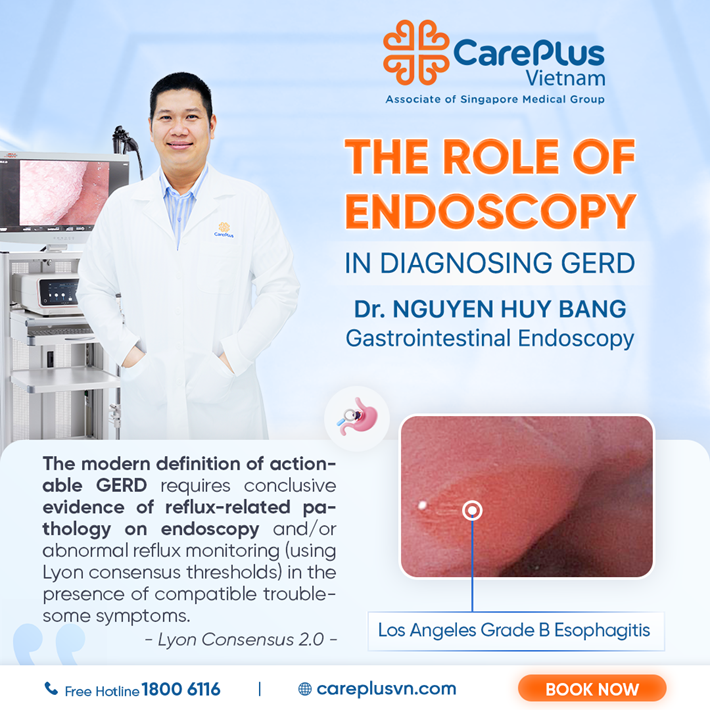
🔹 Severe esophagitis (grades B, C, D) based on the Los Angeles Classification:
ㆍ Grade B: Mucosal breaks longer than 5mm that do not extend between the tops of two mucosal folds.
ㆍ Grade C: Mucosal breaks that extend between the tops of two or more mucosal folds but involve less than 75% of the esophageal circumference.
ㆍ Grade D: Mucosal breaks involving at least 75% of the esophageal circumference, which can cause strictures or lead to serious complications.
🔹 Complications of chronic reflux:
ㆍ Barrett’s esophagus (confirmed by biopsy) – a condition that increases the risk of esophageal cancer if not detected and treated early.
ㆍ Esophageal stricture.
👉 When these lesions are found, GERD can be diagnosed with high certainty without requiring further testing.
⭐ Identifying risk factors for GERD:
🔹 Hiatal hernia: A condition where abdominal organs, such as the stomach, move up into the chest cavity, making acid reflux more likely.
🔹 Assessing mucosal changes: Endoscopy combined with biopsy helps evaluate the extent of mucosal alterations.
⭐ Supporting clinical suspicion when combined with symptoms and pH monitoring:
In some cases, endoscopy may show only mild esophagitis (grade A) or no obvious lesions. In these situations, additional specialized tests such as 24-hour esophageal pH monitoring, along with the patient’s symptoms, are needed for diagnosis.
⭐ Ruling out GERD and screening for other digestive diseases:
When an upper GI endoscopy shows completely normal results with no signs of inflammation or mucosal damage, and physiological tests such as pH monitoring and impedance are also within normal limits, GERD can be ruled out with high confidence.
In such cases, doctors will rely on remaining clinical symptoms to identify other possible digestive causes and develop a more appropriate treatment plan for the patient.
💌 Upper GI endoscopy is a crucial first step in diagnosing GERD, helping to identify the underlying cause and guide appropriate treatment strategies.
🌟 If you’re experiencing symptoms such as heartburn, difficulty swallowing, or suspect you may have GERD – do not overlook this important diagnostic step!
👉 Explore CarePlus gastrointestinal endoscopy services here.
Take proactive steps to protect your digestive health today!
References:
This content was compiled based on the second edition of the Lyon Consensus published in Gut.bmj.com.
The Lyon Consensus is an internationally recognized expert consensus document that provides updated guidelines from leading experts in the field of gastroenterology, particularly regarding GERD.